Research topics
Research topics span a diverse range of fields, offering insights into both theoretical and practical applications. From cutting-edge technology and medical advancements to social sciences and environmental studies, research drives innovation and addresses global challenges. By exploring these topics, we expand our understanding and improve the quality of life.
The challenges and opportunities of digital cloud computing in the delivery of healthcare services in Ethiopia
This study aims to understand the current state of cloud computing in Ethiopia. The analysis focuses on three factors that determine the implementation of cloud computing. First, organizational (top leadership’s management strategy and hospital readiness); second, environmental or external issues ( regulations and standards); and third, technological factors (complexity, relative advantage, and compatibility). The analysis is based on a systematic literature review of high-quality peer-reviewed journal articles, conference publications, online databases, and case studies conducted during the period September/October 2019 in Debre Berhan City, some 57 miles Northeast of Addis Ababa and Finote Selam Hospital in Bahir Dar, about 210 km North of Addis Ababa, during the first week of January 2022. Organizational systems theory is applied to describe the Ethiopian healthcare delivery system, which is dual with manual and electronic methods in capturing, processing, and disseminating medical data. The Ethiopian healthcare system is hierarchical, with significant organizational barriers. It lacks government policy or guidelines for electronic medical health and operates in an environment that limits the growth and development of the electronic healthcare delivery system. Electronic healthcare is limited to specific hospitals lacking interoperability, and the government has shut down the internet in large parts of the country to support its war effort. The study’s findings suggest that the implementation of cloud computing is currently at a stalemate due to organizational and managerial barriers and an ongoing civil war that has decimated the already fragile healthcare system. The infusion of cloud computing technology is considered an alternative to leapfrog the Ethiopian healthcare delivery system since the country’s healthcare infrastructure has been largely destroyed in the last six years. A successful implementation of cloud computing requires an adaptive management strategy that focuses on creating value for healthcare providers and patients. Such a management strategy is known as digital transformative leadership (Schiuma et al., 2024). It is dynamic, involves stakeholders, and incorporates management and quality metrics to gauge progress.
Introduction
This study aims to analyze the major barriers to implementing cloud computing in Ethiopia and propose a management strategy to address some of the challenges. The International Organization for Standardization (IOS) and the International Electro-technical Commission (IEC) defined cloud computing as “a paradigm for enabling network access to a scalable and elastic pool of sharable physical or virtual resources with self-service provisioning and administration on demand” (Miyachi, 2018, p. 8). Figure one presents the conceptual framework of cloud computing in healthcare. Cloud computing addresses two significant challenges of the healthcare delivery system – it enhances healthcare performance and reduces the cost of data storage by making service available on demand. Cloud computing enables hospitals to provide healthcare services at a lower price by streamlining administrative processes, reducing paperwork, and automating tasks (Ciarli et al., 2021). Cost reduction comes in two forms. First, hospitals do not have to develop a massive data infrastructure for storage, maintenance, and processing. Secondly, payment is made only for services used, usually on a pay-as-you-go basis (Mujinga & Chipangura, 2011). Cloud computing can be deployed through public, community, private, or hybrid models. The private models provide greater control for hospitals or healthcare providers. Cloud computing can be deployed as Software-as-a-service (SaaS), Platform-as-a-service (PaaS), or Infrastructure-as-a-Service (IaaS). Hospitals and healthcare providers have greater hardware/software control for IaaS. Cloud computing technologies have significantly increased in developing countries after COVID-19 (Alashhab et al., 2021). However, many hospitals in Africa lack the organizational and management structure to support the implementation of cloud computing (Matchaba, 2019).
Figure 1: Conceptual framework of cloud computing in healthcare
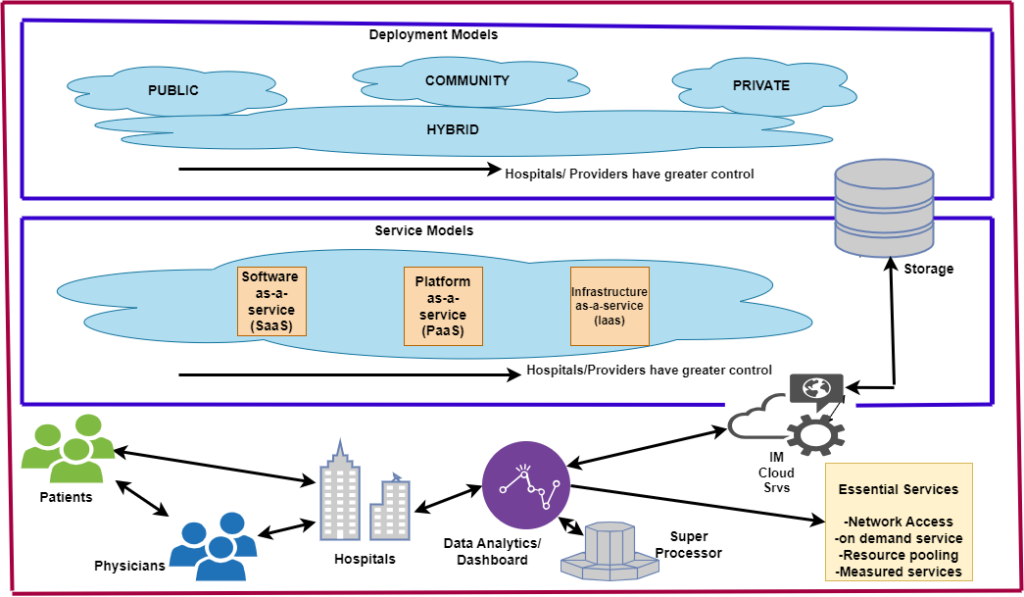
As Figure 1 illustrates, cloud computing enables patient-to-doctor and doctor-to-doctor communication. Patients benefit from doctors’ comprehensive approach to providing treatment. Doctors benefit from the development of an effective clinical decision support system (CDSS) that enables them to perform a wide range of activities, such as vaccination coverage, follow-up treatment outcomes, etc. In general, a CDSS can be used to assess the efficacy of a healthcare system by considering the impact of various health policies and practices ( Antonio, 2014).
The current state of cloud computing in Ethiopia
This analysis applies organizational systems theory to understand the Ethiopian healthcare delivery system. Organizational systems theory considers the whole system and the relationships of its parts rather than focusing on just isolated parts that make up the system (Kast & Rosenzweig, 1972). The theory emphasizes the need to understand the system’s components and their interrelationship in understanding the potential for introducing technological innovation and its likely outcome. Furthermore, the theory helps to understand processes, identify inefficiencies, improve quality of care, evaluate policy options, and enhance decision-making capabilities (Flood & Carson, 2013; Clarkson et al., 2018).
The goal of the Ethiopian healthcare system is “to promote the health and well-being of the society through providing and regulating a comprehensive package of health services of the highest possible quality equitably” (MOH, n.d.). The Ethiopian healthcare system combines manual and electronic healthcare data collection systems, leveraging both paper-based and electronic tools to streamline workflows, enhance communication, and provide better patient care. The healthcare system is hierarchical, with Ministry of Health (MOH) oversight being the highest level of decision-making. MOH designs policies and provides guidelines. In 2015, MOH developed the Health Sector Transformation Plan, which established the Information Revolution (IR), which aims to create an evidence-based decision-making capability by improving clinical data collection, analysis, and dissemination process (PATH, 2019). IR also underscores the need for cultural and attitudinal changes regarding data management and dissemination (FMOH, 2016). In the same year (2015), the Ethiopian Data Use Partnership (DUP) was created to establish a standardized Health Management Information System, eHealth architecture, HIS governance, and improved data use ( PATH, 2019). MOH also established the HMIS (Health Management Information System) unit, which is in charge of recording, managing, and disseminating health data. It has decentralized the management of the public health system to the regional health bureaus and implemented a mobile-based national digital electronic Community Health Information System (eCHIS) to capture data on health extension programs and other community-level services (EMH, n.d.). The degree to which this policy was implemented has not yet been fully analyzed.
Figure 2: Illustration of Ethiopia’s dual health informatics system
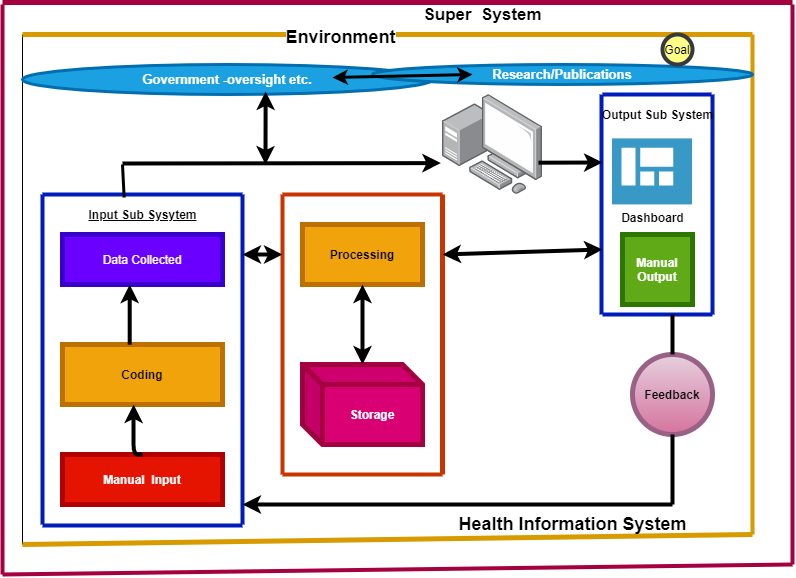
As explained in the previous section, the healthcare delivery system is hierarchical, and the lowest level or subunit is a woreda hospital or clinic. These units collect a wide range of data (input) and generate daily, monthly, and annual reports. In particular, they collect longitudinal data on five broad categories: (1) Family planning, antenatal care, delivery, safe abortion, PMTCT; (2) EPI, vaccine wastage rate, child health and illness management; (3) LBW, GMP, SAM screening, VAS, deworming and IFA; (4) ART by regimen, newly started and retention; and (5) Malaria, VIA, diabetes, hypertension, and cardiovascular. The Hospital also collects socio-demographic data. Nevertheless, “the implementation and diffusion of eHealth technology in Ethiopia is still in its infancy” (EMH, 2019, p.10). In recent years, it has introduced DHIS-2 Tracker, an extension of the DHIS-2 platform. “The Tracker shares the same design concept as the overall DHIS-2. The DHIS-2 Tracker is a powerful HMIS tool for following up on health programs and sharing critical clinical health data across multiple health facilities” (Hlaing & Zin, 2020, p.15). DHIS-2 Tracker can make several types of EMR analysis possible. The manually inputted data is transformed into a digital data record system by transcribing it into Excel or the DHIS-2. The coding or processing step is sometimes simple and sometimes very complex. Several factors, such as shortage of trained personnel, lack of standardization, etc., contribute to the complexity or challenges of transforming manually recorded data from paper to electronic database. The system produces (output) medical reports that physicians and medical staff apply for decision-making. These reports are used internally by physicians and medical staff and sent to the next higher level. The system has a feedback loop to ensure that the processing is performing as expected and informs the design and operation of the subsystems and inputs.
According to the findings of the case studies, the Bahir Dar Finote Selam Hospital applies electronic health records (EHR) for storing patient information, scheduling appointments, and accessing clinical data while utilizing manual methods for patient registration, scheduling, referral, and other tasks that are better suited to paper-based processes. Finote Selam Hospital has an EMR system, Abay CHR (Connected Health Record), a stand-alone electronic data collection system that does not interface with another system. The process of patient data collection both at Bahirdar’s Finote Selam and Debre Birhan is dual – manual and electronic. A patient’s first encounter is with the Triage, where the degree of urgency and the order of treatment are determined based on the severity of the illness. This screening unit separates severe cases, such as bleeding, car accidents, etc., from the less severe cases for immediate urgent care. The non-urgent cases will be referred to the recording unit for registration and treatment. The recording unit also collects socio-demographics, dates, treatments received, etc., and assigns a unique patient identifier number for every patient. The patient identifier is a 16-digit field: the first three digits of the patient identifier are designated for location, followed by three digits for the institution (clinic, Hospital, etc.) identifier. This, in turn, is followed by three fields for ownership (private, Government), and the last four digits are designated to identify the particular patient. It is important to note that the patient identifier is unique to the particular Hospital and has no relevance outside the Hospital. Clinical data is collected by clinicians (Nurses and Doctors) once the patient receives treatment, including service begin/end date, primary and secondary diagnosis applying ICD-10 codes, types of discharge (alive, dead, etc.), medical insurance status, etc. These data will be entered in Excel and transferred to an electronic system such as DHIS. DHIS (district health information system) is a “health information management system – developed through a global collaboration led by the University of Oslo and offered free of charge as a global public good” (Hlaing & Zin, 2019). At Finote Selam, electronic medical records (EMR) are accessible to all medical staff. Every department – maternity, surgery, etc.- has a morning session to review the previous day’s activities from the EMR dashboard. According to the medical director at Finote Selam, the primary purpose of the morning session is to review the Hospital’s clinical activities and prioritize the activities of the particular day. Further analysis is required to understand the process and measures to ensure data integrity.
Regarding organizational structure, both hospitals that have been studied are managed by a board of directors who make strategic decisions and oversee the Hospital’s operations. The board of directors has appointed a Medical Director, who oversees the medical staff and ensures the delivery of quality healthcare services. Medical directors in both hospitals play a significant role in decision-making related to medical policies and procedures. Medical directors oversee the operation of the Hospital’s departments, such as maternity, internal medicine, etc. Each of these departments is led by the department head, who is responsible for managing the department’s operations, supervising the medical staff, and ensuring the quality of care. The Hospital’s administrative and support staff directly report to the board of directors. The IT department that operates EMR and supports admissions and billing also reports directly to the board of directors.
The challenges of cloud computing in the context of the Ethiopian healthcare system
Ethiopia has implemented several eHealth technologies such as SmartCare, mobile ENAT messenger, maternal interactive voice record (IVR), and health management information system (HMIS) over the years (Ahmed et al., 2020) to fulfill WHO’s guidelines. WHO’s vision of 2020 developed a global strategy that improves healthcare for everyone, everywhere, by accelerating the development and adoption of appropriate, accessible, affordable, scalable, and sustainable person-centric digital health solutions (Canton, 2021; WHO, 2021). In 2015, Ethiopia’s healthcare infrastructure was far below what the WHO recommended as the optimal number of doctors, nurses, medical technicians, and healthcare facilities required to serve the population (WHO, 2016). There has been a serious setback in the last six years as the infrastructure crumbled due to a lack of government interest and the social conflict that has erupted in almost all parts of the country. Manyazewal et al. (2021) analyzed the factors that determine the adoption of digital health technologies in Africa, tracking Ethiopia as a critical node. They observed disconnection among critical stakeholders and a lack of a supportive environment, such as electricity and dependable internet services, as major barriers to adopting health informatics technology. The findings of this study collaborate with their conclusion. Health data is also collected by the Central Statistics Agency (CSA) and the Ethiopian Nutrition and Health Research Institute (NHRI), a specialized autonomous agency in the Ministry of Health, which collects data on public health emergencies. There is no coordination among the different government agencies. The country lacks a national health IT policy. As a result, there are no guidelines or procedures to ensure the quality of data being collected. The lack of national policy and standards that govern the development and implementation of electronic health records (EHRs) could result in systems from various vendors not being interoperable.
The economic paralysis and the extended civil war in several regions of the country have further degraded the already fragile healthcare system. A civil war engulfed the country since 2020, and according to international organizations such as the Red Cross, the meager health infrastructure is being destroyed (Icrc, 2023; GanaWeb, 2023). The Government has shut down the internet, and there is no cloud computing without the internet. The civil conflict has destroyed existing health infrastructures in war-affected areas of the country, particularly in Amhara, Tigray, and western Oromia regions. The insecurity in the regions and the lack of transportation have greatly affected the provision and utilization of health services. Cloud computing depends entirely on internet service, and Internet disconnection is a significant problem in Ethiopia. Internet connection is continuously interrupted as the result of the civil war and conflict that engulfed the country and the warring factions’ deliberate destruction of development infrastructures.
Some approaches for a successful implementation of cloud computing
Several works of literature on cloud computing identified (i) senior management support and (ii) organizational structure as essential factors in determining the adoption of cloud computing (Aceto & Pescape, 2020; Amron et al., 2019). Health organizations must implement a technology-focused management approach that considers future demand and scaling capabilities to transition to cloud computing (GeeksforGeeks, 2021). This requires the development of dynamic decision-making capabilities, which is facilitated by increased capacity in accessing real-time data, leading to efficient resource management and cost savings. The Ethiopian healthcare system has a hierarchical organizational structure where decision-making is concentrated at the highest level, and multiple levels of approval are required for the adoption and implementation of cloud computing. The hierarchical management structure is usually resistant to technology-induced changes (McGrath & McManus, 2021). The hierarchical structure of the Ethiopian healthcare sector is less conducive to a technology-focused management approach, which requires hospitals to quickly adjust to ever-changing market conditions (McGrath & McManus, 2021). Senior management decides on the development model (who owns the cloud – public, private, or hybrid) and the delivery model (hardware/software – IaaS, PaaS, or SaaS). Implementing such decisions requires reorganizing the current hierarchical management structure to establish an interdisciplinary, agile, and adaptive management team. It is challenging to be agile in a hierarchical setup, and there are several reasons for this. Decision-making is centralized at the top level of management, and technical and administrative staff lack the authority to quickly adjust to changing conditions. Maintaining established processes and power dynamics can be the primary concern. However, health institutions in Ethiopia can overcome the challenges of hierarchal arrangements by implementing appropriate management strategies.
Researchers have identified senior leadership and management support that embraces the concept of digital management and organizational structure as essential factors in determining the adoption of cloud computing (Kohnke, 2017). Administrators and managers must combine traditional and dynamic leadership to successfully implement cloud computing in a hierarchical administrative setup. Leaders must combine dynamic decision-making capabilities that are agile, flexible, and adaptive to change while embracing traditional leadership principles, such as leading from the middle and supporting each team member by removing organizational barriers, identifying performance shortfalls, correcting deficiencies, and capitalizing on lessons learned (Graffeo, 2019). Successful leaders are profoundly humble, know their limitations, and simultaneously show the way and make big decisions. Digital transformative leaders must be technology-savvy and possess digital expertise. Furthermore, healthcare managers are implementing cloud technology because they deal with technological challenges and legal, cultural, and organizational barriers. The infusion of digital technology against this background could exacerbate the gap in healthcare services unless positively managed. The essential element of a technology-focused management strategy is understanding the Hospital’s capacity in terms of patients treated, bed size, patient/doctor ratio, and its scaling capabilities (GeeksforGeeks, 2021). Furthermore, it is prudent to implement cloud computing in a few hospitals, learn from the experience, and upgrade it to full-fledged implementation. The following steps are recommended to achieve an organizational structure that facilitates a successful implementation of cloud computing.
First, carefully determine the type of cloud computing that meets the health organization’s needs and determine its advantage in terms of its cost and benefit.
Second, a management strategy should be implemented that restructures the organization to make it more agile and adaptable for digital transformation. This can be achieved by reducing the number of hierarchical levels, decentralizing decision-making, and promoting greater collaboration among employees.
Third, explicitly consider expanding access to healthcare and reducing disparities in healthcare services as management’s goal, and regularly monitor, evaluate, and identify bottlenecks. Successful cloud computing management requires leadership that creates a shared vision by participating everyone on the upper leadership ladder, not just a few.
Fourth, embrace training and continuous learning as critical tools for managing cloud computing technologies in the age of globalization since the rate of change is fast. Leaders of health organizations that adopt cloud computing must see themselves as life-long learners.
Cloud computing is expected to bring operational efficiency that reduces medical and administrative errors, streamlines patient information management, improves communication with medical providers, improves access to care, reduces readmission, and increases patient participation and patient satisfaction. It also has the potential to improve financial performance by reducing costs and increasing revenue. Management must introduce indicators to gauge the outcome of cloud computing. The following are management and quality metrics that management can adopt.
Management metrics:
1. Employee Engagement: Metrics such as turnover rate and employee productivity assess employee engagement, motivation, and commitment within the Hospital.
2. Quality and Performance: Metrics such as defect rate, error rate, and customer satisfaction are considered in the erection surveys to measure the performance and quality of products or services provided by the organization.
3. Innovation and Adaptability: Metrics related to research and development investment, new product launches, and market share help assess the organization’s ability to innovate, adapt to changing market conditions, and reduce waste.
4. Employee Development and Succession Planning: Metrics like training and development hours, promotion rates, and talent retention indicate the Hospital’s focus on employee development and succession planning. Training and continuous learning are critical tools for managing cloud computing technologies in the age of globalization since the rate of change is fast and oftentimes discontinuous and unpredictable. Leaders of health organizations that adopt Cloud computing must see themselves as lifelong learners (Canlas, 2022).
5. Ethics and equity. Metrics that measure the reduction of disparities in healthcare services, such as between urban and rural communities or the have and have-not.
Quality metrics:
Quality metrics are also important to consider for the successful implementation of cloud computing. A hospital with a quality management plan is better positioned to implement quality improvement initiatives, and there is a positive relationship between quality management practices and organizational performance (Nguyen et al., 2018). The following are some general metrics that health organizations transitioning to cloud computing may consider. Cloud-based healthcare organizations can develop quality metrics based on priorities and quality management frameworks.
1. First-time resolutions- Measure or track the number of times issues are resolved in the first interaction with patients.
2. Error or defect rate- Track the number of errors or defects in the cloud computing process.
3. Response time- Track the time it takes to resolve issues that patients or customers raise.
4. Compliance rate- Track non-compliance rate. Transitioning to cloud computing can be challenging, as can compliance with government regulations.
Conclusion
This study analyzed the major barriers to implementing cloud computing in Ethiopia and proposed a management strategy to address some of the challenges faced in implementing the technology. Organizational systems theory was applied to explain the Ethiopian healthcare delivery system, which is a dual system of collecting and processing data both manually and electronically. Ethiopia’s healthcare infrastructure is far below what the WHO recommended as the optimal number of doctors, nurses, medical technicians, and healthcare facilities required to serve the population. The analysis identified organizational, environmental, and technological barriers that impede the implementation of cloud computing. The ongoing civil war that engulfed the country during the last six years has further degraded the already fragile healthcare delivery system as health facilities in the Amhara, Oromia, Tigri, and Afar regions have become military targets. Cloud computing is particularly relevant in addressing the disparities created by the devastation of the civil war in the regions. It has the potential to transform the Ethiopian healthcare delivery system by providing a flexible, cost-effective, and secure platform for analyzing and sharing medical data. It can bridge the gap by providing telemedicine and digital health solutions to devastated and war-torn areas. In general, cloud computing leapfrogs healthcare services in areas without fully developed infrastructure. Cloud computing
transforms a healthcare delivery system by providing a flexible, cost-effective, and secure platform for analyzing and sharing medical data. It has encouraged collaboration and enabled doctors to provide better care. Cloud computing is considered an alternative to providing essential services such as network access, on-demand access, resource pooling, etc. The enhanced decision-making capabilities help improve the healthcare system’s efficiency (Zeadally & Bello, 2021). The holy grail for successful digital transformation is building the capacity to meet continuously changing health needs. Management must make a paradigm shift in its approach to address existing health needs and identify emerging trends. A management strategy considering future demand and scaling capabilities was recommended to implement cloud computing successfully. A series of management and quality metrics were developed to gauge the progress of cloud computing.
References
Aceto, G., Persico, V., & Pescapé, A. (2020). Industry 4.0 and health: Internet of Things, big data, and cloud computing for healthcare 4.0. Journal of Industrial Information Integration, 18
https://www.sciencedirect.com/science/article/abs/pii/S2452414X19300135
Ahmed, M. H., Bogale, A. D., Tilahun, B., Kalayou, M. H., Klein, J., Mengiste, S. A., & Endehabtu, B. F. (2020). Intention to use electronic medical record and its predictors among health care providers at referral hospitals, north-West Ethiopia, 2019: using unified theory of acceptance and use technology 2 (UTAUT2) model. BMC Medical Informatics and Decision Making,20(1), 1-11.
Alashhab, Z. R., Anbar, M., Singh, M. M., Leau, Y. B., Al-Sai, Z. A., & Alhayja’a, S. A. (2021).
Impact of coronavirus pandemic crisis on technologies and cloud computing applications. Journal of Electronic Science and Technology,19(1).
Amron, M. T., Ibrahim, R., Bakar, N. A. A., & Chuprat, S. (2019). Determining factors
influencing the acceptance of cloud computing implementation. Procedia Computer Science, 161, 1055-1063.
https://www.sciencedirect.com/science/article/pii/S1877050919319271
António Ferreira Rodrigues Nogueira dos Santos, M., Tygesen, H., Eriksson, H., &
Herlitz, J. (2014). Clinical decision support system (CDSS)–effects on care quality. International Journal of Health Care Quality Assurance, 27(8), 707-718.
Canlas, C. L. M. (2022). The effectiveness of project management credentials and integrated project management implementation on IT project management success [Doctoral dissertation, University of the Cumberlands].
Canton, H. (2021). World Health Organization—WHO. In The Europa Directory of International Organizations 2021 (pp. 370-384). Routledge.
Ciarli, T., Kenney, M., Massini, S., & Piscitello, L. (2021). Digital technologies, innovation, and skills: Emerging trajectories and challenges. Research Policy, 50(7), 104289.
Clarkson, J., Dean, J., Ward, J., Komashie, A., & Bashford, T. (2018). A systems approach to
healthcare: from thinking to practice. Future Healthcare Journal, 5(3), 151.
DHIS2. (2019). University of Oslo health information system program.
https://docs.dhis2.org/2.24/en/user/html/ch27.html)
EMH (n.d.). Ethiopia Ministry of Health www.moh.gov.et/ ; www.moh.gov.et/fmhcaca; www.pfsa.gov.et
Flood, R. L., & Carson, E. R. (2013). Dealing with complexity: an introduction to the theory and application of systems science. Springer Science & Business Media.
FMOH (2015). Ethiopian Federal Ministry of Health (FMOH). Health Sector Transformation Plan 2015/16–2019/20 (2008–2012 EFY). https://www.globalfinancingfacility.org/sites/gff_new/files/Ethiopia-health-system-transformation-plan.pdf.
Gana Web. (2023). Five killed in Ethiopia after drone strike hits ambulances (ghanaweb.com).
GeeksforGeeks. (n.d.). Cloud management in cloud computing. https://www.geeksforgeeks.org/cloud-management-in-cloud-computing/aud
Giordano, C., Brennan, M., Mohamed, B., Rashidi, P., Modave, F., & Tighe, P. (2021). Accessingartificial intelligence for clinical decision-making. Frontiers in digital health, 3.
Graffeo, A. (2018). Leading science and technology-based organizations: Mastering the fundamentals of personal, managerial, and executive leadership. CRC Press.
Hlaing, T., & Zin, T. (2020). Organizational factors in determining data quality produced
from health management information systems in low-and middle-income countries: a systematic review. Health Informatics, 9(4), 10-5121.
Icrc. (2023). Ethiopia: Healthcare crisis in Oromia exacerbated by massive
displacement. International Committee of the Red Cross (ICRC, org).
https://www.icrc.org/en/document/ethiopia-healthcare-crisis-oromia-exacerbated-massive-displacement
Kast, F. E., & Rosenzweig, J. E. (1972). General systems theory: Applications for organization and management. Academy of Management Journal, 15(4), 447-465.
Kohnke, O. (2017). It’s not just about technology: The people side of digitization. Shaping the digital enterprise: Trends and use cases in digital innovation and transformation, 69-91.
Manyazewal, T., Woldeamanuel, Y., Blumberg, H. M., Fekadu, A., & Marconi, V. C.(2021).
The potential use of digital health technologies in the African context: a systematic review of evidence from Ethiopia. NPJ digital medicine, 4(1), 1-13.
Matchaba, P. (2019, August). How to start a digital healthcare revolution in Africa in 6 steps.
World Economic Forum. https://www.weforum.org/agenda/2019/08/6-ways-digital-technology-can-transform- healthcare-in-africa/
McGrath, R., & McManus, R. (2021, May-June). Discovery-driven digital. Harvard Business Review.
MOH. (n.d.). Ethiopia Ministry of Health. Mission, vision, and objectives. (moh.gov.et).
https://www.moh.gov.et/mission-vission-objectives
MOH. (2019). Ethiopia Ministry of Health. www.moh.gov.et/
MOH. (2016). Ethiopian Federal Ministry of Health. Information Revolution Roadmap. Addis Ababa, Ethiopia.
Miyachi, C. (2018). What is “Cloud”? It is time to update the NIST definition? IEEE Cloud computing, 5(03), 6-11. https://web.archive.org/web/20190306204414id_/http://pdfs.semanticscholar.org/cbb4/4eca5afb5901b1a95fd8522528f9e0da7851.pdf
Mujinga, M., & Chipangura, B. (2011, December 5-7). Cloud computing concerns in developing economies. 9th Australian Information Security Management Conference, Edith Cowan University, Perth Western Australia.
https://doi.org/10.4225/75/57b5486bcd8c8
Nguyen, M. H., Phan, A. C., & Matsui, Y. (2018). Contribution to quality management
practices to the sustainability performance of Vietnamese firms. Sustainability,10(2). https://doi.org/10.3390/su10020375
PATH. (2019). Coordinating digital transformation: Ethiopia.
Schiuma, G., Santarsiero, F., Carlucci, D., & Jarrar, Y. (2024). Transformative
leadership competencies for organizational digital transformation. Business Horizons.
World Health Organization. (2016). Health workforce requirements for universal health coverage and sustainable development goals. Human Resource for Health Observers Series No. 17.
http://www.who.int/hrh/resources/WHO_GSHRH_DRAFT_05Jan16.pdf?ua=1.
World Health Organization. (2021). Global strategy on digital health 2020–2025; Licence:
CC BY-NC-SA 3.0 IGO World Health Organization: Geneva, Switzerland.
https://www.who.int/docs/default-source/documents/gs4dhdaa2a9f352b0445bafbc79ca799dce4d.pdf.
Zeadally, S., & Bello, O. (2021). Harnessing the power of Internet of Things-based connectivity to improve healthcare. Internet of Things, 14.
